Abstract
Background: There has been tremendous focus on reducing the impact of healthcare disparities in the treatment of cancer. We have previously demonstrated that healthcare disparities exist in patients undergoing treatment for acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). The purpose of this study was to present outcomes for African American and White patients stratified by disease risk (ELN 2017 cytogenetic and molecular classification) to illustrate healthcare disparities with respect to the biological characteristics of disease.
Patients & Methods: We analyzed 214 patients that underwent treatment for AML from January 2016 to December 2021 at VCU Massey Cancer Center. Patients with intermediate and adverse-risk AML were analyzed, whereas those with favorable risk were excluded due to low sample size precluding meaningful statistical analysis. Within both categories, patients were sub-stratified by self-reported race. Baseline demographics were obtained, including age, performance status, and medical insurance type, as well as disease characteristics, including molecular profiling, cytogenetic risk, doses of induction regimens, response, and survival. Patients were considered evaluable for response if there was a bone marrow biopsy following a minimum of 28 days of treatment. The event for calculating the overall survival (OS) was the date of death with censoring at the date of last contact.
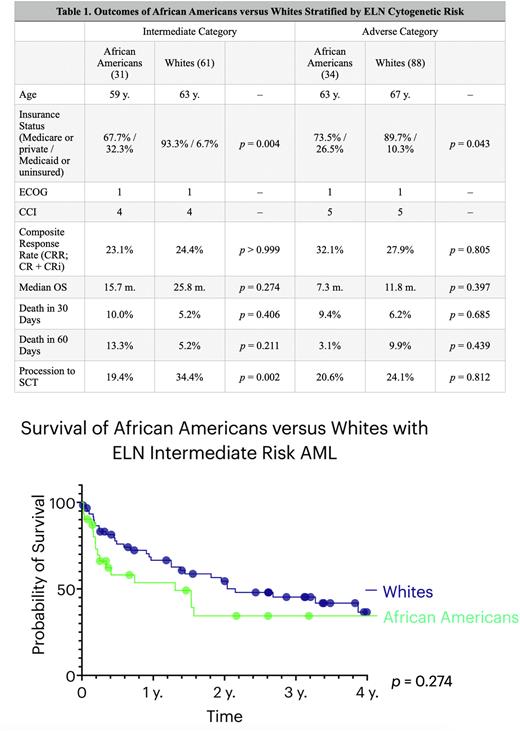
Results: The intermediate-risk category consisted of 92 patients, 31 (33.7%) African American and 61 (66.3%) White. The median ages for African Americans and Whites were 59 and 63 years, respectively, and the median ECOG was 1 while the median Charlson Comorbidity Index (CCI) score was 4 in both cohorts. A total of 67.7% of African Americans had private insurance or Medicare compared to 93.3% of Whites (p = 0.004).At the time of the post-induction marrow, the composite response rate (CRR; CR + CRi) was 23.1% and 24.4% for African Americans and Whites, respectively. The median OS was 15.7 months for African Americans and 25.8 months for Whites (p = 0.274). Rates of death within 30 and 60 days of induction were increased by 12.9% overall in African Americans but did not reach statistical significance (p = 0.406; p = 0.211). Whites were significantly more like to receive SCT than African Americans (34.4% versus 19.4%, p = 0.002).
The adverse category consisted of 122 patients, 34 (27.9%) African Americans and 88 (72.1%) Whites. The median ages of African Americans and Whites were 63 and 67 years, respectively, and the median ECOG and CCI scores were similar between cohorts at 1 and 5, respectively. Significantly fewer African Americans had private insurance or Medicare (73.5%) compared to 89.7% in the White cohort (p = 0.043). The CRR was 32.1% for African Americans and 27.9% for Whites and the median OS was 7.3 months versus 11.8 months for the respective cohorts (p = 0.397). The combined rates of death within 60 days of induction were 12.5% for African Americans and 16.1% for Whites. Progression to SCT numerically favored the White cohort at 24.1% compared to 20.6% in African Americans.
Conclusions: African American and White patients with AML appear to have similar baseline disease characteristics and performance status, although self-identified White patients were significantly more likely to have private insurance or Medicare. Despite similar response rates among those with intermediate-risk AML, African Americans are numerically more likely to experience death within 60 days of induction compared to Whites, although these findings did not reach statistical significance. Whites are also significantly more likely to receive SCT for intermediate-risk disease. The median OS numerically favors Whites in both intermediate and adverse risk cohorts. These findings suggest that structural healthcare disparities, including access to insurance and SCT, are pervasive in the treatment of AML, resulting in African Americans experiencing increased rates of death and reduced survival.
Disclosures
Maher:BMS: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal